Commentary by Joe Vipond, Julia M. Wright, and Dan Furst
It’s time for our society to admit that we’ve made a mistake and change course. The COVID-is-mild experiment, despite the wishing and the hoping, has been a tragic failure. We aren’t just accepting ongoing hospitalizations and deaths to protect the economy, but also ignoring the social and economic costs of continuing high levels of acute infections. Worse still are more cases of Long COVID, a condition that takes many people entirely out of the workforce. And with every wave, the staffing attrition worsens.
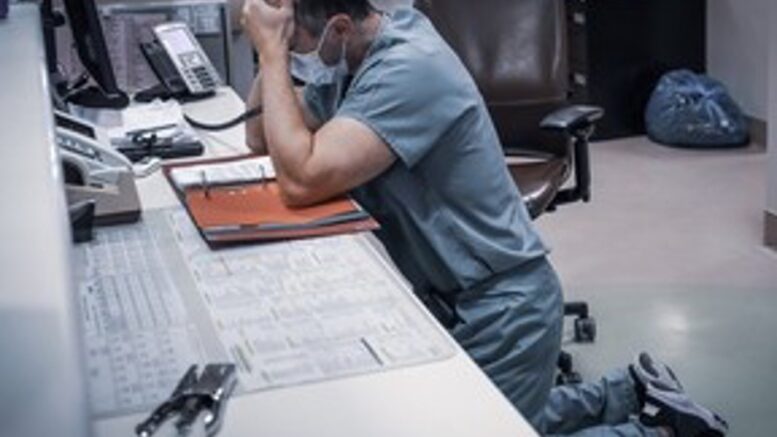
We’re all tired. Even if we’re not sick, we’re covering for sick co-workers, staying home and caring for sick family members and worrying about what’s next. But pandemics are hard and being tired doesn’t change that.
Unlike previous pandemics, though, we have tools for control. We can test and vaccinate; we can reduce transmission by wearing respirator-style masks and improving indoor air quality; and we have better treatments. But our leaders surrendered to the virus.
And to make giving up look reasonable, they avoided certain uncomfortable facts. The silence over Long COVID is particularly deafening. We already saw something similar in the 2002-04 SARS-CoV-1 pandemic. Nearly 30 percent of health-care workers in a 2010 study who had survived SARS “had not returned to work two years after illness onset.”
So it’s no surprise that in our current pandemic we are also seeing long-term illness. Some have challenging but not debilitating effects, such as a chronic cough, or loss of taste and smell. For others, the effects are debilitating, including crushing fatigue or “brain fog” that affects their daily lives—even their ability to return to jobs or school. Long COVID is a significant risk for all age groups, and it’s clear that it’s significantly harming younger working-age adults.
We’ve all seen the headlines about staffing shortages — hospitals, schools, warehouse workers, ferry workers, restaurant staff, and on and on. A recent Quebec study found that “between six and 10 per cent of the province’s health-care workers have experienced long COVID.” A British Medical Association study found that 18 per cent of physicians with Long COVID had symptoms so severe that they could no longer work. This is what attrition looks like.
Vaccination seems to reduce the risk of Long COVID, but fewer people are keeping up to date. In the meantime, people continue to get (re)infected, further increasing the risk —and that’s where the policy of inaction is especially devastating. We were told to get back out there for the economy, but how can the economy withstand endless cuts to our human capital? What price will we pay for allowing this much illness, this much long-term health damage, year after year? Two per cent of the adult population unable to function at work? Five per cent? Ten per cent? Shouldn’t we hit the brakes now?
Our public health and political leaders can start by saying: “It is now settled science that COVID is airborne, and that means we know how to reduce transmission”—universal masking in health-care facilities for the foreseeable future; improve ventilation and filtration in schools and other public spaces; reinstate monitoring and reporting of infections; set thresholds for when we reinstate masks and other protections to avoid the recurrent waves of infections.
Tell people it is worthwhile to avoid getting infected and that there are simple things they can do to reduce their risk of acute and prolonged illness.
Prioritizing the economy over health will sink both. We’ve learned a lot from the past four years. We have the tools to do so much better.
Dr. Joe Vipond is an emergency physician in Calgary, the co-founder of Masks4Canada and ProtectOurProvinceAB, and a member of the John Snow Project.
Julia M. Wright FRSC is a professor and George Munro Chair of Literature and Rhetoric in the Department of English at Dalhousie University, and her research includes work in Health Humanities.
Dan Furst is a lawyer in Calgary and a member of Masks4Canada.
Source: Calgary Herald, Dec 07, 2023